What to expect post transgender bottom surgery?
Missing the Crowning Glory: Hair is how you can gain in back
January 25, 2023Regrowth After Traction Alopecia
March 18, 2023As someone who is exploring gender change treatment and surgery, you may be wondering about the options available to you. One important aspect of gender transition is “bottom surgery,” which refers to surgical procedures that alter the genitals and other reproductive organs. These procedures can include vaginoplasty for transgender women, phalloplasty for transgender men, and metoidioplasty for non-binary individuals. Each individual’s needs and goals are unique, and it’s essential to work with a skilled and experienced surgeon who can help you understand the benefits, risks, and potential outcomes of these procedures. It’s also important to have a strong support system in place, both before and after surgery, as the physical and emotional recovery process can be challenging. Overall, while gender transition can be a long and difficult journey, bottom surgery can be an important step in achieving a more comfortable and authentic sense of self.
Male to Female Bottom Surgery:
As you continue to research gender transition options, you may be specifically interested in male to female (MTF) transgender genital surgery. While vaginoplasty is one of the most well-known procedures for MTF individuals, there are actually several other surgeries that may be involved in a complete transition.
Vaginoplasty: One of the most important procedures for MTF transgender individuals is vaginoplasty, which involves creating a functional and aesthetically pleasing vagina. This procedure can involve various techniques, depending on the individual’s goals and anatomy. Some of the most common methods include using skin and tissue from the penis and scrotum to create a vaginal canal, and using a labiaplasty to create labia.
Labiaplasty: is a procedure that involves creating labia, typically from the same skin and tissue used to create the vaginal canal. The goal is to create labia that look and feel like those of a cisgender woman.
Clitoroplasty: is a procedure that involves creating a functional clitoris, typically using the glans of the penis. The goal is to create a clitoris that is sensitive to stimulation, allowing the individual to experience sexual pleasure.
Orchiectomy: is a surgical procedure that involves the removal of one or both testicles, also known as the testes. This procedure is typically performed on transgender women as part of their gender transition. The testicles are the primary source of testosterone, the male sex hormone, and removing them can reduce or eliminate the effects of testosterone on the body, such as the growth of facial and body hair, and the deepening of the voice. It is important to note that after orchiectomy, individuals will need to take hormone replacement therapy (HRT) to maintain feminizing effects.
Female to male bottom surgery:
If you relate more to a male trapped in a female’s body, you may be looking to change your appearance and sex to male. In that case you may require to undergo FTM bottom surgery in addition to other surgeries and hormone treatment. The goal of FTM genital surgery is to create a functional and aesthetically pleasing penis.
FTM transgender genital surgery, also known as “bottom surgery,” refers to a range of surgical procedures that can help transgender men achieve a more masculine genital appearance and function.
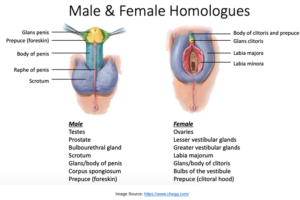
Metoidioplasty: One of the most common procedures is metoidioplasty, which involves releasing the ligaments that hold the clitoris in its original position and then using the newly exposed tissue to create a functional penis. This procedure can involve various techniques, depending on the individual’s goals and anatomy. Some of the most common methods include using the clitoris and surrounding tissue to create a penis, and using a labiaplasty to create a scrotum.
Phalloplasty: Another procedure is phalloplasty, which involves constructing a functional penis. This is a complex and multi-stage procedure that can take several months to complete. The surgical techniques vary and can include using skin and tissue from the thigh or forearm to construct the penis, or using a flap of skin from the abdomen. It’s important to note that the success rate of phalloplasty is lower than other gender reassignment surgeries, and it’s also not always possible to achieve full functionality of the penis.
Hysterectomy: Another procedure that is often performed as part of FTM transition is a hysterectomy, which is the surgical removal of the uterus and the cervix. This procedure is typically performed to remove the organs that are no longer needed after the transition.
Oophorectomy: Oophorectomy is the surgical removal of one or both ovaries, which are the primary source of estrogen, the female sex hormone. This procedure is typically performed as part of a complete hysterectomy.
Vaginectomy: It’s also possible for transgender men to have vaginectomy, which involves removing the vagina. However, this is a complex and multi-stage procedure that is not always successful and is rarely performed.
Post-operative care:
It’s important to note that these procedures are considered “bottom surgery” as they are related to the genitals. Bottom surgery is usually a final step in the transition process, following hormone therapy and other treatments.
The success rate of bottom surgery is generally high, but it depends on the skill and experience of the surgeon, and the individual’s anatomy and goals. It’s important to work closely with a skilled and experienced surgeon to determine the best course of action for you.
After bottom surgery, it’s important to follow a careful post-operative care plan, which may include wound care, physical therapy, and hormone therapy. You will also need to avoid sexual activity for a period of time, to allow for proper healing.
As with any surgery, there are risks associated with bottom surgery, including bleeding, infection, and complications related to anaesthesia. Additionally, the procedure can be difficult to reverse, so it’s important to consider the risks carefully before making a decision.
It’s important to understand that each individual’s transition journey is unique, and the best course of action will depend on your own goals, anatomy, and overall health. It’s crucial to work closely with a skilled and experienced surgeon and a multidisciplinary team of healthcare professionals to determine the right course of action for you.
As for the question of fertility, it may not possible for individuals who have undergone bottom genital surgery to conceive or impregnate. However, some transgender persons may choose to freeze their sperm or eggs before undergoing surgery, so that they have the option to use assisted reproductive technologies in the future.
Overall, it’s important to understand that each individual’s transition journey is unique, and the best course of action will depend on your own goals, anatomy, and overall health. It’s crucial to work closely with a skilled and experienced surgeon and a multidisciplinary team of healthcare professionals to determine the right course of action for you.
What one should expect in life post-op transgender genitalia surgeries?
After undergoing transgender genital surgery, individuals can expect to experience a range of physical and emotional changes.
Long recovery period: On the physical side, individuals can expect to have a significant recovery period. This period can vary depending on the type of surgery, but in general, individuals will need to take time off work or school, and may need assistance with daily activities for several weeks. In some cases, individuals may experience pain, swelling, and bleeding in the surgical area, and will need to follow a specific wound care regimen. It’s also common for individuals to experience changes in sexual function and sensation
Emotional mess: On the emotional side, individuals can expect to experience a range of emotions related to their surgery and recovery. Many individuals report feeling a sense of relief and satisfaction after surgery, as well as a greater sense of comfort and authenticity in their bodies. However, it’s also common for individuals to experience feelings of anxiety, depression, and stress related to the recovery process and the changes they are experiencing. It’s important to have a strong support system in place, both before and after surgery, as the recovery process can be challenging. This can include friends, family, a therapist, and a support group.
It’s also important to note that the surgical result may not be exactly what one expects, and revision surgeries may be needed. In addition, individuals may need to continue hormone therapy, and may need to make lifestyle changes such as adjusting clothing and grooming habits.
Overall, individuals should expect a recovery period of several weeks, possibly longer, and a range of physical and emotional changes. With the right support and care, most individuals are able to adjust to their new bodies and move on with their lives.
How successful are gender reassignment surgeries in terms of quality of life, in terms of looks and functionality, and their overall health which is governed by hormones?
The success of bottom surgeries, also known as gender reassignment surgeries, can vary depending on a number of factors, such as the skill and experience of the surgeon, the individual’s anatomy and goals, and the individual’s overall health.
In general, the success rate of Male-to-Female (MTF) genital surgery, such as vaginoplasty, is considered to be high in terms of both aesthetics and function. The goal of the surgery is to create a functional and aesthetically pleasing vagina, and most individuals who undergo the surgery are satisfied with the results.
Similarly, Female-to-Male (FTM) genital surgery, such as metoidioplasty and phalloplasty, also has a high rate of success in terms of aesthetics. The functional success of the procedures may vary depending on the individual’s anatomy and the surgical technique used. In general, metoidioplasty has a higher rate of functional success than phalloplasty.
In terms of overall health, individuals who undergo gender reassignment surgeries will need to continue hormone therapy, which can have an impact on their overall health. Hormone therapy can have both positive and negative effects on an individual’s health, depending on their unique circumstances. Some individuals may experience side effects such as weight gain, acne, and changes in blood pressure, cholesterol, and glucose levels. However, most of these side effects can be managed with proper care and monitoring by a healthcare professional.
In terms of quality of life, studies have shown that individuals who undergo gender reassignment surgeries report significant improvements in their quality of life, including increased satisfaction with their bodies, improved sexual function and satisfaction, and reduced symptoms of gender dysphoria.
It’s important to note that these procedures are complex surgeries and require a high level of skill and experience from the surgeon. The success rate is also dependent on the individual’s own goals and expectations, and it’s not always possible to achieve full functionality of the genitals, depending on the individual’s anatomy and the procedure performed.
Additionally, the success rate of these surgeries can be affected by the patient’s compliance with post-operative care and follow-up visits, so it is important to be aware of that as well.
Additional tips for better and long-term results post-op transgender genitalia surgery include:
- Follow-up with your surgeon: It’s important to attend all follow-up appointments with your surgeon to ensure proper healing and to address any concerns you may have.
- Physical therapy: Depending on the type of surgery you have had; your surgeon may recommend physical therapy to help improve healing and regain strength and function in the surgical area.
- Be patient with healing process: Healing can take time, and it’s important to be patient and allow your body to heal properly.
- Avoid smoking and excessive alcohol consumption: These habits can impede the healing process and may increase the risk of complications.
- Hormone therapy: As part of the transition process, it is important to continue hormone therapy as directed by your healthcare provider, as it can have a significant impact on the overall healing process.
- Mental Health Support: it’s important to have a strong support system in place, both before and after surgery, as the recovery process can be challenging. This can include friends, family, a therapist, and a support group.
- Be realistic about the outcome: it’s important to have realistic expectations about the outcome of the surgery, and understand that the results may not be exactly what you expect.
- Choosing an experienced surgeon: the experience of the surgeon plays asignificant role in the success of the surgery, so it’s important to choose a surgeon who has experience and expertise in performing transgender genitalia surgeries. Make sure to research the surgeon’s qualifications, training, and experience, and ask to see before-and-after photos of their previous patients.
- Follow a healthy diet and lifestyle: Eating a healthy diet and maintaining a healthy lifestyle can improve your overall health and well-being, and help promote healing after surgery.
- Be aware of the risks and complications: As with any surgery, there are risks and complications associated with transgender genitalia surgeries. It’s important to be aware of these risks and to discuss them with your surgeon before making a decision.
By following these tips, individuals can improve their chances of achieving better and long-term results after transgender genitalia surgery. It’s important to remember that each individual’s journey is unique, and it’s essential to work closely with a qualified and experienced surgeon and a multidisciplinary team of healthcare professionals to determine the best course of action for you.
FAQs
No, it isn’t. It may be possible to implant prosthesis but, it is impossible to recreate a penis or a uterus.
The rate of success depends on a lot of factors like the patient’s satisfaction. A study indicates that about 94% to 100% of patients who undergo the surgery are happy with the results. Only about 1% of them regret the decision.

